Little ones explore the world with their hands and mouths, and while you do your best to keep them safe, it's wise to prepare for unexpected moments. This choking first aid guide will help you understand the signs of choking. But it's best paired with basic life support (BLS) training from the Philippine Red Cross or from American Heart Association-accredited institutions for an even greater benefit.
How to Recognize the Signs of Choking
Before you jump into action, it's key to know the signs of choking and how different it is from gagging. It’s also important to know that the way a baby shows they’re in distress might look a little different from how an older child reacts. Here’s what to watch out for:
Gagging (natural reflex)
This is the body (whether baby or young kid) trying to prevent an object from blocking their airway. You might see forceful coughing, watery eyes, or even a little vomiting. If they’re gagging but still coughing, let them try to clear the object while you watch closely.
Mild choking (partial airway blockage)
In this case, some air is still getting through, and your child's airway is only partially blocked.
- An older child will likely cough to try to dislodge the object. They might still be able to make sounds, speak, cry, or make other sounds between coughs.
- A baby will also cough (though it might sound less forceful than an older child’s) and can still cry, sputter, or make other gurgling or gasping sounds.
Encourage your child to keep coughing. Stay with them and monitor the situation to make sure it doesn't worsen.
Severe choking (a life-threatening emergency)
This is when you need to immediately perform choking first aid because little to no air is getting through. Look for these urgent signs in babies and older children:
- Your child can't cry, cough effectively (any cough will be weak, silent, or absent), or make any sound at all.
- Their skin, lips, and nails can rapidly turn blue or dusky due to a lack of oxygen.
- You might hear high-pitched, whistling noises if any air squeezes past the blockage, or more commonly, no sound.
- With older kids, you might also see a panicked look, and they may clutch their throat—the universal sign for choking.
Choking First Aid for Babies (1 Year Old and Below)
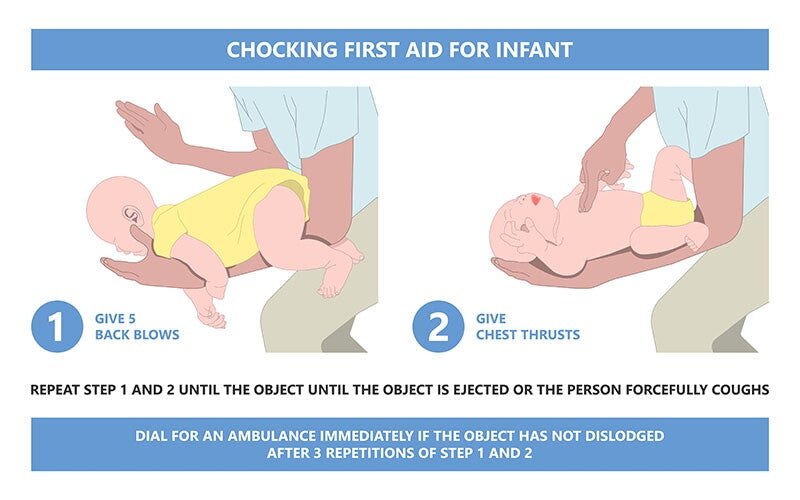
If a baby is alert but showing signs of severe choking, perform the following steps:
1. Get help.
When a child is choking, every second is precious. Your immediate goals are to get medical help on its way and start first aid.
Shout for help if someone else is nearby. Tell them to call the emergency hotline (911) and also try the Philippine Red Cross at 143 to request an ambulance, clearly stating that a child is choking. While they’re making that call, begin the first aid steps.
If you’re alone, your first move is to start first aid immediately using the steps below for a full two minutes—this typically involves about five cycles of back blows and chest thrusts. After these vital first few minutes, then call 911 or 143.
2. Position your baby.
In a sitting or kneeling position, lay your baby face down on your forearm, supporting their head and jaw with your hand. Keep their head lower than their chest, resting your forearm on your thigh for support.
3. Deliver five firm back blows.
Give five firm back blows between your baby's shoulder blades with the heel of your other hand.
4. Reposition for chest thrusts.
Supporting the head and neck, turn your baby face-up on your forearm or lap, keeping their head lower than their chest.
5. Deliver five quick chest thrusts.
Place two fingers in the center of your baby's chest (below nipple line). Give five quick, downward chest thrusts.
6. Repeat the cycle.
Repeat five back blows and five chest thrusts until the object is out, your little one breathes or coughs forcefully, or becomes unresponsive.
First Aid for Children (1 Year Old and Up)
If your child is over a year old is alert and showing signs of severe choking, shout for help immediately and begin first aid. If someone is nearby, have them call 911 or 143.
If you’re alone and your child is conscious, try to dislodge the object first before calling emergency services. Use the following steps below:
1. Ask, "Are you choking?"
If they nod yes or can’t speak, tell them calmly that you're going to help them.
2. Deliver five firm back blows.
Stand or kneel behind your child. If they’re small, lean them forward slightly, supporting their chest with one hand. Give five firm back blows between their shoulder blades with the heel of your other hand.
3. Perform five abdominal thrusts.
Stand or kneel behind your child, wrapping your arms around their waist. Make a fist; place the thumb side against their abdomen (above navel, below breastbone). Grasp your fist with your other hand. Deliver quick, upward and inward abdominal thrusts (also known as the Heimlich maneuver). Each thrust should aim to lift the diaphragm and expel the object.
4. Repeat the cycle.
Continue alternating between five back blows and five abdominal thrusts until you dislodge the object and your child can breathe, speak, or cough forcefully on their own, or they become unconscious.
What to Do If Your Child Becomes Unconscious
If your child becomes unresponsive at any point, whether before you started first aid or even while you are giving back blows or abdominal thrusts, you need to get help immediately. If someone is with you, have them call 911 or 143 and state that an unconscious child was choking.
If you’re alone, call either of these numbers right away. Put your phone on speaker to talk to the dispatcher while you attend to your child. Emergency dispatchers are trained to guide you.
Watch the video below for recommended first aid steps for an unresponsive child:
Seek Medical Attention After First Aid
Even if you successfully dislodge the object and your child seems fine, they should go to a doctor or the ER immediately. The choking itself or abdominal thrusts could cause internal injury.
Medical resources like NIH’s StatPearls confirm that even after symptoms resolve, a retained object or airway issues like swelling can still exist, requiring a check-up.
Report any of the following symptoms to the doctor, even if you were able to remove the object:
- A persistent cough or wheezing
- Difficulty swallowing or painful swallowing
- Drooling more than usual
- Pain in the throat or chest
- Unusual fatigue, or if your child just doesn't seem like themselves.
Choking First Aid "Don'ts" for Children
When your child is choking, knowing what not to do is just as important as knowing the proper steps to take, especially in a high-stress moment. Here's what to avoid when performing choking first aid on a child.
Blind finger sweeps
Don't put your fingers in your child's mouth unless you can see and easily remove the object. Blindly sweeping with your fingers can push the object deeper into the airway, worsening the situation or causing injury.
Heimlich maneuver in babies
Don't perform the Heimlich maneuver (abdominal thrusts) on your baby if they're under 1 year old. Use back blows and chest thrusts instead. Abdominal thrusts can cause internal injuries to babies.
Turning a child upside down
Don't pick up and turn your child upside down when they're choking. This is ineffective and can also cause further harm or injury.
Back blows while your child is upright
Don't bang your child's back while they are upright. The correct position for back blows is with the child leaning forward or, for babies, face-down along your forearm or thigh. Avoid excessive force, too, because it can break ribs or damage internal organs, especially in children.
Giving food or drink to dislodge an object
Don't encourage the child to drink water or eat anything to "wash down" the object. This can worsen the obstruction and is not a safe or adequate response.
Safety Tips to Prevent Choking
Preventing choking is your first and best defense. This is particularly true for young children, as a review of prevention strategies shows that most choking injuries in children aged 0 to 3 are food related. Follow these tips to keep your child safe.
- Supervise mealtimes. Ensure they sit down; do not run, play, or lie down with food, especially if they eat solids.
- Cut food into small pieces. According to the Australian Journal of General Practice, nuts, hard raw vegetables like carrots, and round berries are common choking hazards.
- Teach safe eating habits. Encourage older children to chew thoroughly, take small bites, and not talk or laugh with a full mouth.
- Keep small objects out of reach. Regularly check for coins, buttons, toy parts, marbles, pen caps, and other small items, ensuring a baby-proof your home.
Now that you know what to do if your child is choking, you can calmly and confidently act in an emergency. Mentally walk through these steps regularly. Better yet, consider enrolling in a certified first-aid and CPR course or other DOLE-approved first-aid training providers. Your quick response, guided by the correct knowledge of choking first aid, can make all the difference.
Connect with other parents on the ParentTeam Moms and Dads Facebook group and discuss baby safety and choking first aid tips to help your child fast.
References
Alzahrani, K., N. A. Alzahrani, S. M. Alghamdi, H. A. Alshamrani, H. A. Alghamdi, and M. I. Barnawi. "Safety Practices in Al-Baha: A Cross-Sectional Study on Parental Awareness of Child Choking Events." Cureus 16, no. 6 (June 2024): e62100. Accessed May 21, 2025. https://doi.org/10.7759/cureus.62100.
American Red Cross. "Child & Baby CPR." American Red Cross Training Services. Accessed May 20, 2025. https://www.redcross.org/take-a-class/cpr/performing-cpr/child-baby-cpr.
Davies, Hannah, and Sarra VglNT. "Paediatric inhaled airway foreign bodies." Australian Journal of General Practice 48, no. 4 (April 2019): 223–27. Accessed May 21, 2025. https://www1.racgp.org.au/ajgp/2019/april/paediatric-inhaled-airway-foreign-bodies.
Duckett, Scott A., Michael Bartman, and Ryan A. Roten. "Choking." In StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing, January 2025. Last updated September 19, 2022. Accessed May 21, 2025. https://www.ncbi.nlm.nih.gov/books/NBK499941/.
Karišik, Milenko. "Foreign Body Aspiration and Ingestion in Children." Acta Clinica Croatica 62, Suppl 1 (2023): 105–12. Accessed May 21, 2025. https://doi.org/10.20471/acc.2023.62.s1.13.
Mayo Clinic Staff. "Choking: First aid." Mayo Clinic. Last modified May 24, 2024. Accessed May 20, 2025. https://www.mayoclinic.org/first-aid/first-aid-choking/basics/art-20056637.
Newfoundland and Labrador, Department of Health and Community Services. "Food Choking Hazards." Healthy Eating for Babies Age 6-12 Months: A Guide for Parents and Caregivers. Last modified October 4, 2024. Accessed May 20, 2025. https://www.gov.nl.ca/healthyeating/baby/building-healthy-eating-habits/food-choking-hazards/.
New York State Department of Health. "Choking Prevention for Children." Last revised February 2022. Accessed May 20, 2025. https://www.health.ny.gov/prevention/injury_prevention/choking_prevention_for_children.htm