
Monkeypox in the Philippines: Everything Parents Need to Know
Concerns about monkeypox in the Philippines have surged again following the Department of Health's confirmation of over 50 cases in April 2025 and new infections reported in Davao City in May.
While most Filipinos with mpox have recovered without serious complications, DOH officials urge the public to remain cautious. So, what does the presence of monkeypox, also known as mpox, mean for your day-to-day life?
Here's what you need to know about monkeypox transmission, symptoms, and what you can do to protect your family.
What Is Mpox?
Mpox is an infectious viral disease that can infect humans and animals. According to the World Health Organization (WHO), the cause of mpox is the monkeypox virus (MPXV), which belongs to a group of viruses known as Orthopoxviruses within the Poxviridae family. This family of viruses includes variola (the virus that causes smallpox), cowpox, and vaccinia.
Scientists have identified two distinct genetic groups (or clades) of the monkeypox virus:
- Clade I, which used to be called the Congo Basin clade, has a reputation for causing severe illness and higher death rates.
- Clade II, also known as the West African clade, is typically associated with milder cases and the group of monkeypox viruses that triggered the ongoing global mpox outbreak.
As of June 2025, DOH reports that all confirmed cases of monkeypox in the Philippines belong to clade II.
Monkeypox Symptoms
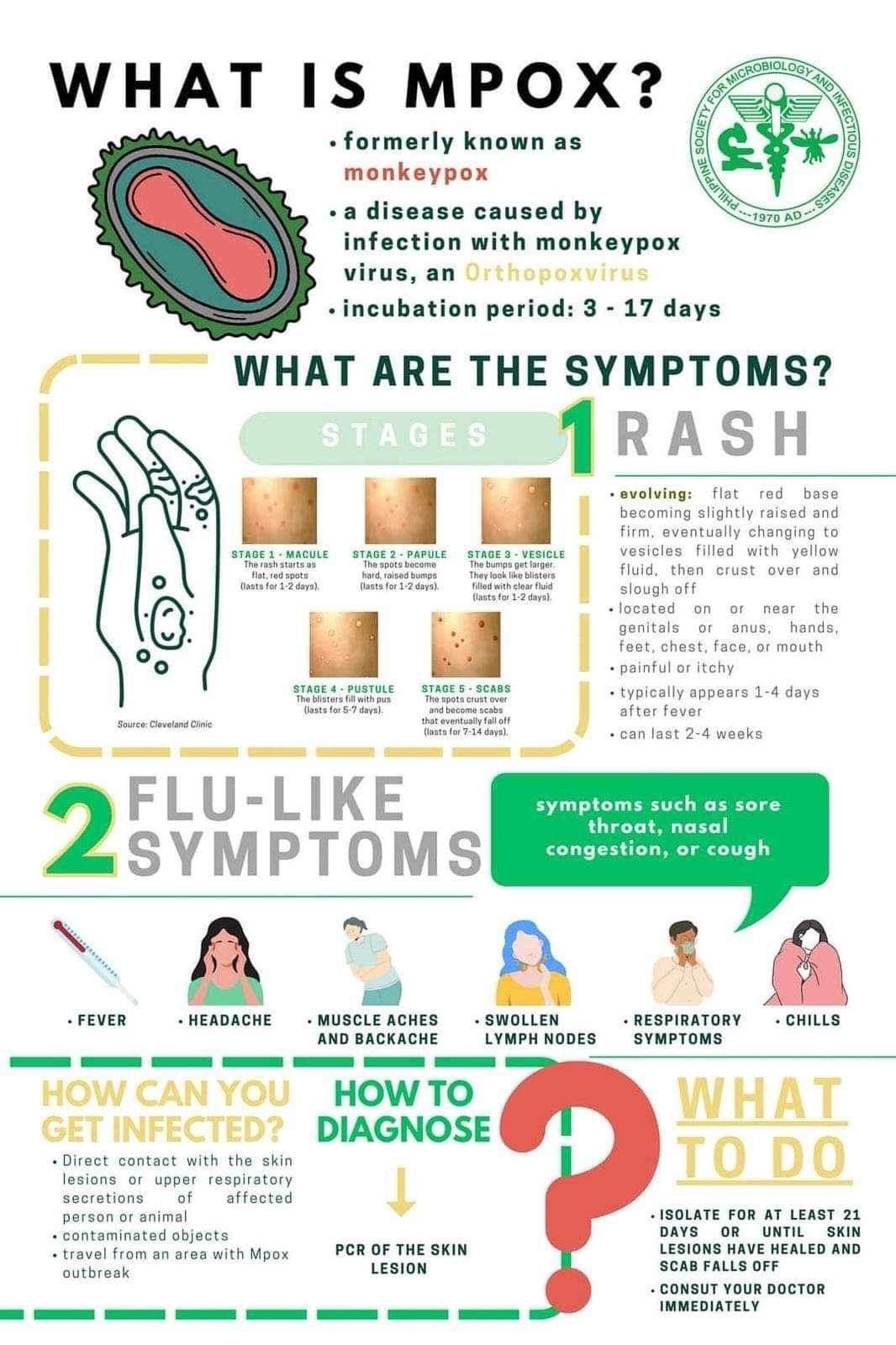
If you become exposed to mpox, the infection enters an incubation period, which can last from three to 17 days. You'll feel completely fine and are not contagious until the mpox symptoms appear.
What often worries health officials about mpox is its symptoms are similar to those of other health conditions. By the time people realize what they have is mpox, they could have unknowingly spread the disease.
You can help prevent the disease by knowing how monkeypox symptoms progress.
Flu-like symptoms
The first signs of mpox often feel like the flu. Common symptoms include:
- Fever
- Headache
- Muscle aches and backache
- Chills and shivering
- Swollen lymph nodes (the glands in your neck, armpits, or groin may swell and feel sore)
- Fatigue or exhaustion
- Sore throat or cough
It's easy to ignore these symptoms, especially when they're mild, thinking you're just coming down with a cold. So, sometimes, people will only think it's not the flu when they notice a skin lesion like a rash.
Rash development
A rash usually develops one to five days later or alongside the flu-like symptoms. However, some people may only experience a rash without any other mpox symptoms.
Monkeypox-related rashes go through the following stages:
- Stage 1: A rash called macule appears. They're flat, red spots that last for one to two days.
- Stage 2: The spots become raised and firm, known as papules. They resemble small bumps and last for one to two days.
- Stage 3: The bumps turn into blisters or vesicles. They're filled with clear fluid and can last for up to two days.
- Stage 4: The blisters now fill with pus and become pustules officially. They last for five to seven days.
- Stage 5: The skin lesions eventually crust over, forming scabs that last for up to 14 days.
The rashes can appear anywhere but often start on the face, then spread to other parts like the hands, feet, chest, mouth, genitals, or anus. They can become painful or itchy. These skin lesions can appear one to four days after a fever and last between two to four weeks.
How Can You Get Infected

If you have mpox, you can't hug or kiss your loved ones to prevent spreading the disease.
Most monkeypox cases are primarily transmitted through direct, skin-to-skin contact rather than casual interactions or passing by someone. WHO reports that mpox mainly spread through sexual contact during the global outbreak that began in 2022. You catch mpox in the following ways:
Person-to-person
- Touching the rash, sores, or body fluids of someone with mpox
- Kissing or other intimate sexual activity
- Breathing in tiny droplets from someone who is infected because you talked with them or they coughed and sneezed in your space
- Touching items like bedding, towels, clothing, or surfaces that have been used by someone with mpox.
- Eating or drinking from the same container as an infected person
If you're pregnant and have the virus, you can pass mpox to your baby in the womb or during birth, which can be dangerous for the baby.
Animal-to-person
Mpox is a zoonotic disease, meaning it can jump from animals to humans. This can happen in several ways:
- Being bitten or scratched by an infected animal
- Handling or touching an infected animal’s blood, saliva, respiratory secretions, or the fluid from their sores
- Hunting, skinning, trapping, cooking, or eating wild animals with mpox
- Touching or being exposed to feces or other waste from infected animals
Mpox isn't as contagious as everyday respiratory viruses, such as the flu or COVID-19, because it's not an airborne disease.
What to Do if You or a Loved One Has Mpox Symptoms

Don't share plates and utensils with someone who has mpox.
Depending on the severity of symptoms, having mpox doesn't always require hospitalization but rather self-quarantine. If a household member, particularly a child, has been diagnosed, follow the doctor's orders. DOH also recommends these at-home care tips:
1. Isolate as much as possible.
If your child or a family member has numerous visible rashes or symptoms, such as coughing, a sore throat, or a runny nose, quarantine them in a separate room to prevent the virus from spreading to other household members.
2. Use gloves when needed.
If you need to touch the rashes (for example, while cleaning them), wear disposable gloves and dispose of them immediately after use.
3. Keep skin covered.
Dress your child (or the person with monkeypox) in long sleeves and pants, and cover any open sores with clean dressings, especially if they’re leaking fluid. This adds a layer of protection for everyone else at home.
4. Hands off the rashes.
It’s tempting, but try to stop your child (or yourself) from scratching the lesions or picking at scabs. Doing so can lead to scarring or, worse, a secondary bacterial infection. Dermatologists suggest keeping fingernails trimmed short to help prevent accidental scratching.
5. Wear masks inside the home.
The person with monkeypox should wear a surgical mask, especially if they have any breathing or throat symptoms. If it’s a child who can’t wear a mask, then you (and others at home) should wear one whenever you're near them.
6. Do not make trips outside.
Stay home for the entire isolation period of at least 21 days or until all the rashes have dried up and healed.
7. Handle waste safely.
Items like used bandages or dressings should go in a separate trash bin, ideally a yellow bag if available. Clean the area before throwing them out.
If a waste collector is picking up your garbage, let them know you have medical waste so they can take proper precautions. Try to avoid throwing this kind of waste into regular landfills.
8. Use separate plates and utensils.
Give the household member with mpox their own set of utensils and plates to help prevent the virus from spreading to others at home
9. Disinfect surfaces
Clean doorknobs, counters, or tables. You can use your regular household cleaning sprays or wipes. Follow the directions on the bottle to ensure they work correctly.
10. Limit visitors.
If someone doesn’t absolutely need to be in your home, especially if they haven’t been exposed, they should hold off on visiting until isolation is over. It’s all about protecting everyone, just in case.
11. Keep some distance.
Family members who aren’t sick should keep their distance from the person with monkeypox as much as possible, even though that’s tough—especially with young kids.
12. Keep pets out of the sick room.
Your furry family members need protection, too! Try to keep pets away from the person with monkeypox to avoid possible transmission.
How to Help Prevent the Spread of Monkeypox
Even if there’s no case in your home, it's still good to know how to help protect your family and your community. Here are some easy-to-follow reminders:
Keep your distance from sick animals.
If an animal looks unwell (or worse, has been found dead), especially in areas where monkeypox has been reported, avoid contact and report it to local authorities.
Don’t touch items used by infected people and sick animals.
That includes bedding, blankets, or other materials they might have come into contact with.
Wash those hands often!
Whether it's with soap and water or an alcohol-based hand sanitizer, clean hands are one of the easiest and most effective ways to prevent mpox from spreading.
FAQs About Monkeypox in the Philippines
Still have questions about monkeypox? This quick FAQ covers additional info from monkeypox treatment to scarring.
Is monkeypox a public health emergency in the Philippines?
No, it isn't. The country has seen cases rise since it recorded its first mpox case in 2022. But DOH says the established mpox response measures are working, including contract tracing and isolation.
In September 2024, 200 possible monkeypox cases were reported, but only 20 were confirmed as mpox. All the confirmed cases in the country so far are from the milder version of the virus (clade II), which doesn't spread as quickly as other infections and has a lower risk of serious illness or death. As of May 2025, the DOH reported fewer mpox cases than the number recorded in 2024.
Do face masks prevent mpox infection?
Local governments in areas like Davao Del Sur and Maasin in Leyte, where mpox has been reported, have required their residents to wear face masks. However, the Philippine Society for Microbiology and Infectious Diseases (PSMID) says "compulsory masking" is not necessary since mpox is not an airborne disease.
Are there vaccines for monkeypox?
Yes, some vaccines help prevent mpox and reduce its symptoms. Monkeypox vaccines include MVA-BN (known as Jynneos in the United States) and ACAM2000 (currently licensed in the U.S. but with restricted use).
However, no monkeypox vaccine has been approved by the Philippine Food and Drug Administration (FDA) for use. So, prevention is really your best protection.
Can monkeypox cause permanent scars?
It's possible. Scratching, rubbing, or picking at monkeypox scars can damage the skin further. It also slows down the healing process and significantly increase the likelihood of permanent scarring. A Journal of the American Academy of Dermatology study shows that 13 people out of 101 mpox cases resulted in visible scarring where the rashes or skin lesions initially appeared.
Do I need to throw away my clothes if I have mpox?
No, you can wash them as you would any laundry. You can add bleach if you want to, but it's not absolutely necessary. But, when you're picking up dirty laundry, wear gloves and a mask to prevent direct contact with germs. And try not to shake the dirty laundry out!
Is monkeypox deadly?
While mpox can become serious and lead to complications, it is rarely deadly, especially the type (clade II) that's causing monkeypox in the Philippines. Most people who get mpox recover fully on their own, often within a few weeks.
Who's the most vulnerable to mpox?
Anyone can get mpox, but certain groups are at higher risk for more serious illness and complications, such as:
- Newborn babies and young children (especially under 1 year old) since their immune systems are still developing.
- Pregnant women who may be at risk of complications like miscarriage or stillbirth if they get infected
- People with severely weakened immune systems, like cancer patients undergoing chemotherapy or people on immunosuppressant medications
- A person with a history of eczema, since the condition makes the skin more vulnerable to severe and widespread rashes
Staying informed and vigilant about monkeypox in the Philippines can help you protect your family. The good news is that, in most cases, mpox clears up on its own. Just keep an eye out for any symptoms, and if you suspect that a member of your household has been exposed, isolate them and contact a doctor immediately. You're not just protecting your family, but you're helping to keep your whole community safe.
Have you or your family experienced mpox? Share how you managed it with the members of the ParentTeam Moms and Dads Facebook group!
References
“Mpox,” n.d. https://www.who.int/news-room/questions-and-answers/item/mpox.
Mpox. “Clinical Features of Mpox,” September 12, 2024. https://www.cdc.gov/mpox/hcp/clinical-signs/index.html.
Mpox. “Interim Clinical Considerations for Use of Vaccine for Mpox Prevention in the United States,” February 14, 2025. https://www.cdc.gov/mpox/hcp/vaccine-considerations/vaccination-overview.html.
Philippine News Agency. “Davao City’s Mpox Cases Rise to 6,” n.d. https://www.pna.gov.ph/articles/1251153.
GMA Integrated News. “DOH: Mpox Cases Actually Dipped in May 2025; Total Cases 911 Since 2024.” GMA News Online, May 31, 2025.









